- Summary
- Symptoms
- Read More
Sesamoiditis is an inflammatory condition of one or both of the sesamoid bones which are located on the plantar (bottom) aspect of the first metatarsal phalangeal joint (1st MPJ or big toe joint.) Sesamoiditis occurs at the articulation of the sesamoid and the overlying 1st metatarsal bone. Sesamoiditis is usually caused by chondromalacia, or softening of the surface cartilage of the sesamoid where it articulates with the 1st metatarsal. As chondromalacia of the sesamoid progresses over time, it will contribute to the onset of osteoarthritis of the articulation of the sesamoid and 1st metatarsal. Sesamoiditis is found equally in men and women. The onset of sesamoiditis is insidious between the ages of 25 and 50 years of age.
Symptoms
Pain specific to the bottom of the great toe joint
Pain site-specific when palpated with a single finger
Minimal edema, erythema or bruising
Pain increased with weight bearing and increased with toe raise
Increased pain with the use of high heels
Description
 Primary sesamoiditis is due to an inflammatory reaction at the articulation of the sesamoid with the plantar surface of the 1st metatarsal head. This inflammation is caused by chondromalacia. Chondromalacia describes softening and progressive degeneration of the articular cartilage. Secondary sesamoiditis is caused by atrophy of the fat pad of the forefoot. Thinning of the fat pad beneath the sesamoid can lead to pain with weight bearing by placing direct pressure on the sesamoid. In this case, there is no chondromalacia found in the sesamoid-1st metatarsal articulation. Although not truly an inflammatory type of problem, pain under the sesamoid that is caused by thinning of the fat pad may also be called sesamoiditis.
Primary sesamoiditis is due to an inflammatory reaction at the articulation of the sesamoid with the plantar surface of the 1st metatarsal head. This inflammation is caused by chondromalacia. Chondromalacia describes softening and progressive degeneration of the articular cartilage. Secondary sesamoiditis is caused by atrophy of the fat pad of the forefoot. Thinning of the fat pad beneath the sesamoid can lead to pain with weight bearing by placing direct pressure on the sesamoid. In this case, there is no chondromalacia found in the sesamoid-1st metatarsal articulation. Although not truly an inflammatory type of problem, pain under the sesamoid that is caused by thinning of the fat pad may also be called sesamoiditis.
The two sesamoid bones are located on the bottom surface of the first metatarsal phalangeal joint. The sesamoids are actually a working part of the 1st MPJ and articulate with the plantar surface of the first metatarsal. The sesamoid bones are an extension of the flexor hallucis brevis (FHB) muscle and give the FHB a greater range of motion and improved lever action at the level of the 1st MPJ. Sesamoid bones are referred to by their location and are called the tibial sesamoid (medial) and the fibular sesamoid (lateral) bones. Tibial and fibular make reference to the bones of the lower leg: the tibia and fibula.
Causes and contributing factors
The underlying cause of primary sesamoiditis is due to osteoarthritis at the sesamoid 1st metatarsal articulation. Contributing factors may include trauma to the joint or a predisposition to osteoarthritis. Contributing factors to secondary sesamoiditis include fat pad atrophy and the use of thin-soled shoes or inappropriate shoes for specific activities.
Differential diagnosis
The differential diagnosis for sesamoiditis includes:
- Arthritis
- Bunion
- Bursitis
- Chondromalacia
- Gout
- Hallux limitus
- Hallus rigidus
- Septic joint (infection)
- Pseudogout
- Sesamoid fracture
- Turf toe
Treatment
Conservative treatment of primary and secondary sesamoiditis consists of limiting activities and padding or "off-loading" of the joint. Off loading refers to taking the weight bearing load off of a particular area by use of a dancer's pad. In the case of sesamoiditis, the off-loading pad should be approximately 1/4" thick with a cut out for the bottom of the 1st MPJ. Should temporary padding help, a prescription orthotic with a similar pad would be indicated. The prognosis of conservative care in cases of sesamoiditis depends upon the stage of chondromalacia found in the sesamoid-1st metatarsal articulation. In early stages, conservative care of sesamoiditis can be quite successful. In advanced stages of chondromalacia, off-loading will ease pain but will not relieve the sharp, shooting arthritic pain of advanced osteoarthritis of the sesamoid-1st metatarsal articulation.
The prognosis of conservative care provided in cases of secondary sesamoiditis caused by fat pad atrophy can be quite good. A cut out pad like a dancer's pad in conjunction with silicone gel cushioning is very successful. Although going barefoot may still be uncomfortable, pain can be relieved while wearing shoes with a dancer's pad.
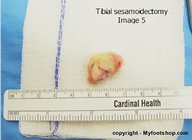
Surgical treatment of sesamoiditis consists of removal of the entire sesamoid bone. Occasionally, planing of the bone, or removing the bottom half of the bone may be a useful surgical procedure. Planing is used less often than total excision due to the fact that planing will weaken the sesamoid and may lead to fractures of the sesamoid post-op. As an alternative to sesamoidectomy, a surgical osteotomy can be performed at the base of the first metatarsal to elevate the head of the first metatarsal. A dorsiflectory wedge osteotomy (DFWO) is a bit more involved than a simple sesamoidectomy. A DFWO takes about 45 minutes to complete and can be performed under local anesthesia with sedation. Recovery requires a non-weight bearing hard cast be worn for 6 weeks following surgery. The following images show a transverse DFWO of the 1st metatarsal base, fixated with monofilament wire. The long-term success of a DFWO is good to excellent.
A sesamoidectomy can be performed on an out-patient basis at a hospital or surgery center. The procedure is performed with local anesthesia and mild sedation. The procedure can be performed in 30 minutes. Most patients are able to bear weight on the foot the same day of the surgery. Sutures are removed at two weeks and a return to full weight bearing begins at 4-6 weeks post-op. The following images show the steps involved in performing a tibial sesamoidectomy. The long-term success of a sesamoidectomy is good to excellent.
Removal of the tibial or fibular sesamoids does not typically affect the normal function of the great toe joint. If a patient has a family history of bunions or currently has a bunion, there will be a tendency to increase the rate that a bunion will form with isolated removal of the tibial sesamoid. By removing the tibial sesamoid, the pull of the FHB muscle will become slightly more powerful through the remaining fibular sesamoid. As a result, this may accelerate fibular (lateral) drift of the great toe and the formation of a bunion. If there is no history of bunions in the family, this may not even become a factor in choosing to excise the tibial sesamoid.
When to contact your doctor
Sesamoid pain that does not respond to conservative care should be evaluated by your podiatrist or orthopedist.
References
References are pending.
Author(s) and date
![]() This article was written by Myfootshop.com medical advisor Jeffrey A. Oster, DPM.
This article was written by Myfootshop.com medical advisor Jeffrey A. Oster, DPM.
Competing Interests - None
Cite this article as: Oster, Jeffrey. Sesamoiditis. https://www.myfootshop.com/article/sesamoiditis
Most recent article update: January 14, 2021.
 Sesamoiditis by Myfootshop.com is licensed under a Creative Commons Attribution-NonCommercial 3.0 Unported License.
Sesamoiditis by Myfootshop.com is licensed under a Creative Commons Attribution-NonCommercial 3.0 Unported License.
Internal reference only: ZoneP5, ZoneM8