How is Morton's neuroma diagnosed? This article is the first of three articles that discuss the symptoms and treatment options for Morton's neuroma.
How is Morton's neuroma diagnosed?
Diagnosing Morton's neuroma begins with a thorough patient history. The questions asked by your health care provider will likely include where the problem is located, the duration of the symptoms, the character of the symptoms, the onset of the symptoms and what methods of treatment you may have tried to date. The history taken by your doctor may seem like a simple way to first evaluate the problem, but the history is actually the single best tool your doctor has to determine whether or not you are suffering from Morton's neuroma. Let's take a look at each of the history questions that we just asked and see how they may provide your doctor with information about a Morton's neuroma.
Where is Morton's neuroma located in the foot?
The location of a Morton's neuroma is most commonly going to be found on the plantar (bottom) aspect of the forefoot. Morton's neuroma is usually found between the third and fourth toes (third intermetatarsal space or third IMS) and to a lesser degree 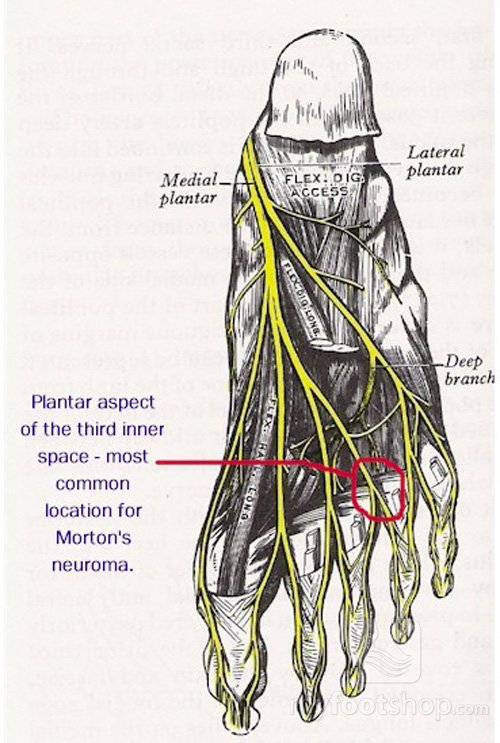 between the second and third toes (second inter-metatarsal space). In my practice, I've found it rare, if ever at all, that I've diagnosed a Morton's neuroma in the first or fourth inter-metatarsal spaces. The reason that Morton's neuroma is so common in the 3rd IMS is due to a unique anatomical adaptation of the digital nerves of the forefoot. In the accompanying image, the branches of the medial plantar nerve and the lateral plantar nerve join into a common digital nerve in the 3rd IMS. This finding is unique to the 3rd IMS. Clinicians believe that this confluence of the two nerves results an the common digital nerve of the 3rd IMS being bound and not able to move and adapt to the motion of the forefoot. As the nerve passes distally to the toes, it passes below the intermetatarsal ligament. It's at this location, adjacent and plantar (below) the ligament that the irritation of the nerve occurs. Therefore, location of the symptoms is very critical in the diagnosis of Morton's neuroma.
between the second and third toes (second inter-metatarsal space). In my practice, I've found it rare, if ever at all, that I've diagnosed a Morton's neuroma in the first or fourth inter-metatarsal spaces. The reason that Morton's neuroma is so common in the 3rd IMS is due to a unique anatomical adaptation of the digital nerves of the forefoot. In the accompanying image, the branches of the medial plantar nerve and the lateral plantar nerve join into a common digital nerve in the 3rd IMS. This finding is unique to the 3rd IMS. Clinicians believe that this confluence of the two nerves results an the common digital nerve of the 3rd IMS being bound and not able to move and adapt to the motion of the forefoot. As the nerve passes distally to the toes, it passes below the intermetatarsal ligament. It's at this location, adjacent and plantar (below) the ligament that the irritation of the nerve occurs. Therefore, location of the symptoms is very critical in the diagnosis of Morton's neuroma.
The duration of the symptoms of Morton's neuroma vary. Many patients find that the symptoms are situational meaning that if they don't wear shoes that irritate the nerve, they have limited symptoms. Due to the situational nature of the symptoms, many patients will describe symptoms that have come and gone for years.
What are the symptoms of Morton's neuroma?
The character of the symptoms of Morton's neuroma is also an important aspect of the history and helps to define the presence of a Morton's neuroma. Patients describe a sensation of walking on a bunched up sock or as if something is in their shoe. Some describe a clicking or popping sensation and other electrical shocks out to the toes. The symptoms increase with the duration of time on the feet and increase with tightness of the shoe on the forefoot. Wider shoes and lower heels result in less severe symptoms. Tighter shoes and higher heels increase symptoms. Symptoms of Morton's neuroma are relieved by rest.
The onset of the symptoms of Morton's neuroma vary. And again, this may be situational. The onset might be abrupt when wearing a pair of heels to a wedding but subside once returning to more casual shoes. In other cases, the symptoms may progressively increase over weeks to months.
How is Morton's neuroma treated?
Treatment methods that you may have tried also matter to your doctor and are an important part of your history. Wider shoes, arch support, and shoe pads can all help your doctor determine whether Morton's neuroma is present or not.
Once your doctor has completed your history, he or she will examine your foot. The clinical symptoms of Morton's neuroma may vary based upon the amount of swelling and size of the nerve. A small Morton's neuroma may come and go based upon the shoes that you wear and the activities that you are involved in. In the case of a smaller Morton's neuroma, the clinical symptoms may be  difficult to elicit upon examination. Your doctor will first feel the bottom of the foot for any sense of a mass between the toes. He or she will then wrap their hand around the forefoot and squeeze while pushing up on the bottom of the foot at the site of the neuroma. In a more advanced case and with a larger neuroma, the patient will feel a snapping or popping sensation in the forefoot. This test is called a Muldier's sign. A positive Muldier's sign results in pain and electrical shock sensations to the toes. Although a positive Muldier's sign (with pain) is pathoneumonic for Morton's neuroma, a Muldier's sign without pain does not necessarily mean that a neuroma requires treatment.
difficult to elicit upon examination. Your doctor will first feel the bottom of the foot for any sense of a mass between the toes. He or she will then wrap their hand around the forefoot and squeeze while pushing up on the bottom of the foot at the site of the neuroma. In a more advanced case and with a larger neuroma, the patient will feel a snapping or popping sensation in the forefoot. This test is called a Muldier's sign. A positive Muldier's sign results in pain and electrical shock sensations to the toes. Although a positive Muldier's sign (with pain) is pathoneumonic for Morton's neuroma, a Muldier's sign without pain does not necessarily mean that a neuroma requires treatment.
Additional parts of the clinical exam may include having you stand, applying weight to the bare foot. In some cases, weight-bearing with a mass such as a neuroma between the toes will result in spreading of the third and fourth toes. This is what some doctors call a victory sign.
Imaging studies are often used to help diagnose Morton's neuroma. X-rays are commonly used to rule out specific conditions that may contribute to forefoot symptoms that may be similar to Morton's neuroma. These conditions include metatarsalgia, arthritis, Freiberg's infraction, foreign body, and previous forefoot trauma. Ultrasound is particularly helpful in imaging Morton's neuroma. Hand held ultrasound may be used to determine the size of the interdigital nerve. If the size of the interdigital nerve is increased, these findings suggest the diagnosis of Morton's neuroma. MRI is used in some cases to diagnose Morton's neuroma but based upon the cost of an MRI, this imaging study is not favored by insurance companies (or patients for that matter, right?)
Another less frequently used diagnostic method used to assess Morton's neuroma is a digital nerve block. Local anesthesia is used to block the nerve in the 3rd IMS. Although this isn't a common diagnostic tool, I'll use this technique if I suspect that the pain may either be in part or completely due to tarsal tunnel syndrome. I won't speak here about tarsal tunnel syndrome, but you may follow the link for more information. Suffice it to say, tarsal tunnel syndrome should be considered within the differential diagnosis of Morton's neuroma.
What is the differential diagnosis of Morton's neuroma?
And lastly, what is the differential diagnosis for Morton's neuroma? A differential diagnosis is a list of conditions that may mimic a Morton's neuroma. We've mentions metatarsalgia, arthritis, Freiberg's infraction, foreign body, prior forefoot trauma, and tarsal tunnel syndrome. Additional considerations in the differential diagnosis for Morton's neuroma include capsulitis and metatarsal stress fractures.
Related blog posts:
Morton's neuroma - history
Morton's neuroma - conservative care
Morton's neuroma - surgical care
Jeff
Medical Advisor
Myfootshop.com
Updated 4/23/2021