- Summary
- Symptoms
- Read More
- Video
Summary
Tarsal tunnel syndrome (TTS) refers to an entrapment of the posterior tibial nerve as it descends from the leg passing through the medial ankle to the foot. This condition was first described by Keck and Lam in 1962.(1,2) The terminal aspect of the posterior tibial nerve (L4-S1 nerve distribution) supplies the motor function to the muscles of the foot and the sensory innervation to the bottom of the foot. Varying degrees of entrapment of this nerve may affect either motor function, sensory function, or both. Tarsal tunnel syndrome may be found unilaterally or bilaterally. Tarsal tunnel syndrome is found equally between men and women.(3,4,5)
Symptoms
- Pain in the medial ankle and plantar foot that increases with duration of weight bearing, pain described as "vise like".
- No pain with initial weight bearing.
- Pain relieved with a long period of rest.
- No swelling, redness or bruising is found.
Description
Tarsal tunnel syndrome occurs on the medial aspect of the ankle, just behind and below the medial (inside) ankle bone. Many of the structures that govern the function of the foot pass through a tunnel in this area referred to as the porta pedis (window of the foot) or tarsal canal. These structures include arteries, veins, nerves, and multiple tendons. As these structures round the inside of the ankle, they are held in place by a broad ligament known as the lacinate ligament. The purpose of the lacinate ligament is to prevent these vital structures from bowstringing or popping out of position with walking or running. The posterior tibial nerve passes through the porta pedis. The posterior tibial nerve is susceptible to problems as it passes deep to the lacinate ligament and abductor hallucis muscle. If for any reason pressure is applied to the posterior tibial nerve, symptoms of tarsal tunnel will occur.

 Testing for tarsal tunnel syndrome with nerve conduction studies and EMG (electromyography) is often imprecise and misleading. The most reliable method of assessing tarsal tunnel syndrome is percussion of the nerve. This test is called a Tinel's sign. Two fingers are used to briskly tap the medial ankle just behind and below the ankle bone (medial malleolus.) An electrical shock sensation is called a positive Tinel's sign and indicates the location of the entrapment. The pictures to the left show the location of the posterior tibial nerve (in green) as it descends the leg behind the inside ankle bone (medial malleolus.) Two common areas of entrapment are found as the posterior tibial nerve passes beneath the lacinate ligament (in pink) and/or the upper margin of the abductor hallucis muscle (dotted line.) The posterior tibial nerve passes deep to the muscle at the dotted line. The margin of the abductor hallucis muscle is the most common location for entrapment of the posterior tibial nerve.
Testing for tarsal tunnel syndrome with nerve conduction studies and EMG (electromyography) is often imprecise and misleading. The most reliable method of assessing tarsal tunnel syndrome is percussion of the nerve. This test is called a Tinel's sign. Two fingers are used to briskly tap the medial ankle just behind and below the ankle bone (medial malleolus.) An electrical shock sensation is called a positive Tinel's sign and indicates the location of the entrapment. The pictures to the left show the location of the posterior tibial nerve (in green) as it descends the leg behind the inside ankle bone (medial malleolus.) Two common areas of entrapment are found as the posterior tibial nerve passes beneath the lacinate ligament (in pink) and/or the upper margin of the abductor hallucis muscle (dotted line.) The posterior tibial nerve passes deep to the muscle at the dotted line. The margin of the abductor hallucis muscle is the most common location for entrapment of the posterior tibial nerve.
The posterior tibial nerve splits into three branches at the level of the medial ankle. A positive Tinel's sign may be positive for all three branches or just one isolated branch. This variation in the Tinel's sign depends upon the level of the entrapment and whether the entrapment is proximal or distal to the triforcation (split) of the nerve into its three branches.
An alternative method of nerve conduction testing proposed by Lee Dellon, MD of Baltimore, MD, uses a device called a pressure specified sensory device or PSSD. This method incorporates two-point discrimination and pressure testing to quantify sensory loss due to nerve entrapments. Use of PSSD testing by clinicians has not been universally accepted.
Causes and contributing factors
There's no universal agreement between clinicians and surgeons as to why tarsal tunnel syndrome occurs. Contributing factors that may cause tarsal tunnel syndrome include trauma to the tarsal canal, varicose veins, bone spurs, and soft tissue tumors such as ganglionic cysts. Other contributing factors include biomechanical instability of the foot caused by pronation (flattening of the arch) and supination (high arch.) Each of these contributing factors ultimately results in compression of the posterior tibial nerve. The site where the nerve is compressed is also called an entrapment.
Differential diagnosis
The differential diagnosis for tarsal tunnel syndrome includes:
Arthritis
Baxter's nerve entrapment
Entrapment, lumbar spine, at the level of L3 to S1
Entrapment, sciatic nerve, beneath the piriformis muscle
Entrapment, posterior tibial nerve, behind the knee
Flexor digitorum longus tendonitis
Gout
Navicular fracture
Nerve tumor
Posterior tibial tendonitis (PTTD)
Sinus tarsi syndrome
Treatment
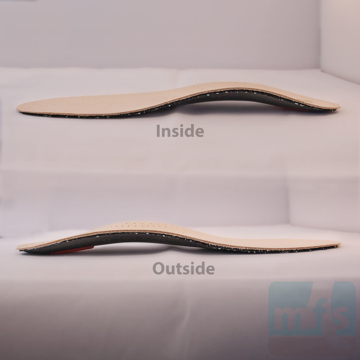
Conservative care for tarsal tunnel syndrome includes injectable cortisone and support of the arch. Many studies have shown that the pronated or flat foot is much more prone to tarsal tunnel syndrome.(6) Arch support has been shown to decrease strain on many of the structures (nerve and tendon) that pass from the leg to the foot through the tarsal canal.
Tarsal tunnel syndrome may be treated surgically with a release of the lacinate ligament and exploration of the tarsal canal with decompression of the posterior tibial nerve deep to the abductor hallucis muscle. Most peripheral nerves are slow to respond to surgical procedures. The recovery period for patients undergoing tarsal tunnel surgery may vary from 3 months to 18 months. The outcome of the procedure varies and seems to depend upon the nature of the entrapment and the damage that the posterior tibial nerve had sustained prior to surgery.
The pictures below show the steps involved in a tarsal tunnel release. Image 1 shows the planned incision line running behind the medial ankle to a level just distal to the upper margin of the abductor hallucis muscle. Dissection is carried down through the subcutaneous space where, in Image 2, we see the lacinate ligament identified. Image 3 shows the lacinate ligament released and direct visualization of the posterior tibial nerve and associated vein and artery. Image 4 shows the posterior tibial nerve isolated. The nerve and surrounding soft tissue is inspected for any visual defects including tumors or evidence of trauma. Image 5 shows the dissection of the Baxter's nerve. Image 6 shows the fibrous tissue that invests the abductor hallucis muscle. The fibrous tissue surrounding the abductor hallucis extends into the porta pedis. A tarsal tunnel release requires dissection of this fibrous tissue into the porta pedis to ensure a complete release.
The calcaneal branch of the posterior tibial nerve may become selectively entrapped as it descends from the tarsal canal to supply sensory innervation to the bottom of the heel. This condition is called a Baxter's nerve entrapment and is an important differential diagnosis in treating heel pain and should always be considered a possibility when treating plantar fasciitis.
When to contact your doctor
Symptoms of tarsal tunnel syndrome that fail to respond to conservative care should be evaluated by your podiatrist or orthopedist.
References
- Lam SJS (1962) A tarsal-tunnel syndrome. Lancet ii:1354–1355.
- Keck C (1962) The tarsal-tunnel syndrome. J Bone Joint Surg A 44:180–182.
- Lam SJS (1967) Tarsal-tunnel syndrome. J Bone Joint Surg B 49:87–92.
- Linsheid RL, Burton RC, Fredericks EJ (1970) Tarsal tunnel syndrome. South Med J 63:1313–1323.
- Takakura Y, Kitada C, Sugimoto K, et al. (1991) Tarsal tunnel syndrome. J Bone Joint Surg B 73:125–128.
- Plast Reconstr Surg. 2009 Oct;124(4):1202-10
Author(s) and date
![]() This article was written by Myfootshop.com medical advisor Jeffrey A. Oster, DPM.
This article was written by Myfootshop.com medical advisor Jeffrey A. Oster, DPM.
Competing Interests - None
Cite this article as: Oster, Jeffrey. Tarsal Tunnel Syndrome. https://www.myfootshop.com/article/tarsal-tunnel-syndrome
Most recent article update: January 15, 2021.
 Tarsal Tunnel Syndrome by Myfootshop.com is licensed under a Creative Commons Attribution-NonCommercial 3.0 Unported License.
Tarsal Tunnel Syndrome by Myfootshop.com is licensed under a Creative Commons Attribution-NonCommercial 3.0 Unported License.
Internal reference only: ZoneM5, ZoneM6,ZoneP2,ZoneR3