- Summary
- Symptoms
- Read More
Summary
Haglund's deformity is the term used to describe an enlargement of the posterior/lateral heel. Haglund's deformity also goes by the name of Haglund's disease and pump bump. Most clinicians agree that Haglund's deformity is formed by rolling of the heel into the heel counter, or rim of the shoe. The development of a pump bump is a reactive bone formation in response to chronic pressure on the heel. Haglund's deformity is common in individuals who wear shoes that have a rigid heel counter such as ice skates or pump heels. Haglund's deformity occurs in patients between the ages of 20 to 60 years. Haglund's deformity is more common in women than in men.
Symptoms
- Enlargement of the posterior/lateral heel
- Pain free when barefoot
- Pain with direct pressure from shoes
Description
The term pump bump is the slang term used to describe Haglund's deformity and was popularized in the mid-fifties when pump high heels were in fashion. The rigid heel counter of the pump applies direct pressure to the enlargement of the heel resulting in pain and an inability to wear pumps.
It's important that Haglund's deformity be differentiated from a very similar problem known as insertional Achilles tendonitis. Haglund's deformity is specific to the posterior lateral heel and does not involve the Achilles tendon.  Haglund's deformity does not hurt when barefoot and is only aggravated by direct pressure from shoes. Insertional Achilles tendinitis, on the other hand, encompasses the entire posterior heel. The pain found with insertional Achilles tendinitis is specific to the onset of gait, such as getting out of bed in the morning or trying to walk after sitting for a short period of time, or both. Achilles tendinitis hurts both with and without shoes. Although both Haglund's deformity and insertional Achilles tendinitis result in enlargement of the posterior heel, it's important to differentiate between the facts that Haglund's deformity is specific to the posterior lateral heel and insertional Achilles tendinitis encompasses the entire posterior heel. This differentiation between Haglund's deformity and Achilles tendinitis will become important when planning a surgical procedure to correct each of these two problems.
Haglund's deformity does not hurt when barefoot and is only aggravated by direct pressure from shoes. Insertional Achilles tendinitis, on the other hand, encompasses the entire posterior heel. The pain found with insertional Achilles tendinitis is specific to the onset of gait, such as getting out of bed in the morning or trying to walk after sitting for a short period of time, or both. Achilles tendinitis hurts both with and without shoes. Although both Haglund's deformity and insertional Achilles tendinitis result in enlargement of the posterior heel, it's important to differentiate between the facts that Haglund's deformity is specific to the posterior lateral heel and insertional Achilles tendinitis encompasses the entire posterior heel. This differentiation between Haglund's deformity and Achilles tendinitis will become important when planning a surgical procedure to correct each of these two problems.
Haglund's deformity is often accompanied by bursitis. In addition to reactive enlargement of the heel bone, chronic pressure to the posterior/lateral heel often results in bursitis of the heel. This particular bursal sac forms between the heel and skin. Inflammation of the bursal sac, called bursitis, can be quite painful and limit an individual’s ability to wear shoes.
Causes and contributing factors
The cause of Haglund's deformity is direct pressure to the posterior lateral heel from a rigid heel counter. Contributing factors include rigid heels such as ice skates, athletic shoes, and pump high heels.
Differential diagnosis
The differential diagnosis for Haglund's deformity includes:
Achilles tendon rupture
Calcaneal fracture
Gout
Insertional Achilles tendinitis
Retrocalcaneal bursitis
Shepard's fracture
Treatment
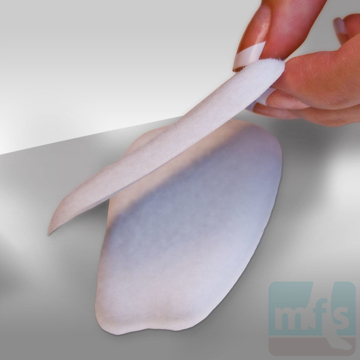
Conservative care of Haglund’s deformity focuses on avoiding direct pressure on the back of the heel. Shoes that have a rigid heel counter should be avoided. Open back shoes like clogs and flip-flops can help by simply decreasing direct pressure to the posterior heel. When closed heel shoes are required, a heel lift can be used to raise the heel above the heel counter.
Use of oral anti-inflammatories and cortisone are not particularly effective if direct pressure to the posterior heel continues. Although anti-inflammatories may help to ease pain, the primary cause of Haglund’s deformity is mechanical due to direct pressure from the shoe. Therefore, the success of anti-inflammatory medication may be limited.
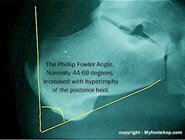 Many Haglund's deformity cases will require surgery. Pre-op evaluation of a Haglund's deformity includes assessment of the heel with a lateral x-ray of the foot. The reactive bone deposit on the posterior heel in a Haglund's deformity can be visualized. As a result, the heel which is normally round in the back becomes square like the head of a tomahawk. This increase in bone on the back of the heel is measured by a radiographic angle called the Phillip-Fowler angle. An increase in the Phillip-Fowler angle suggests hypertrophy of the posterior heel
Many Haglund's deformity cases will require surgery. Pre-op evaluation of a Haglund's deformity includes assessment of the heel with a lateral x-ray of the foot. The reactive bone deposit on the posterior heel in a Haglund's deformity can be visualized. As a result, the heel which is normally round in the back becomes square like the head of a tomahawk. This increase in bone on the back of the heel is measured by a radiographic angle called the Phillip-Fowler angle. An increase in the Phillip-Fowler angle suggests hypertrophy of the posterior heel
Surgical care of Haglund’s deformity focuses on resection of the posterior/lateral bump of the heel. Most cases of Haglund’s deformity can be corrected without displacement of the Achilles tendon from the back of the heel. The advantage of keeping the Achilles tendon intact is that patients are able to ambulate immediately post-op. If the primary problem is insertional Achilles tendinitis, and the Achilles tendon does need to be transposed (moved) during the surgery, patients are placed in a below-the-knee cast for 6-8 weeks to allow for adequate healing of the tendon.
In severe cases of Haglund’s deformity, a Keck and Kelly procedure may be performed. A Keck and Kelly procedure is a wedge resection of the calcaneus that results in the shortening of the calcaneus. A Keck and Kelly procedure would be performed in conjunction with a partial resection of the posterior heel.
Surgical resection of a Haglund’s deformity (without a Keck and Kelly procedure) is performed on an outpatient basis using either a general anesthetic or local anesthesia with sedation. The procedure takes approximately 30 minutes to complete. This procedure is typically performed in the prone position. Healing from this surgery does vary, but most patients are back into a regular shoe at 4-6 weeks following surgery.
When to contact your doctor
Haglund's deformity that fails to respond to conservative care should be evaluated by your local podiatrist or orthopedist.
References
References are pending.
Author(s) and date
![]() This article was written by Myfootshop.com medical advisor Jeffrey A. Oster, DPM.
This article was written by Myfootshop.com medical advisor Jeffrey A. Oster, DPM.
Competing Interests - None
Cite this article as: Oster, Jeffrey. Haglund's Deformity https://www.myfootshop.com/article/haglunds-deformity
Most recent article update: December 10, 2020.
 Haglund's Deformity by Myfootshop.com is licensed under a Creative Commons Attribution-NonCommercial 3.0 Unported License.
Haglund's Deformity by Myfootshop.com is licensed under a Creative Commons Attribution-NonCommercial 3.0 Unported License.
Internal reference only: ZoneP1, ZoneL4, ZoneR2