- Summary
- Symptoms
- Read More
- Video
Summary
The Achilles tendon is the body's single strongest tendon. An Achilles tendon rupture can be partial or complete. A partial rupture, often called a tear, can be a localized (micro) or a longitudinal rupture. A partial or complete rupture of the Achilles tendon is an injury that requires prompt medical attention.
Symptoms
Partial Achilles Tendon Rupture
Insidious or abrupt onset with pain and swelling 2 to 3 centimeters proximal to the insertion of the Achilles tendon into the back of the heel.
Pain is most pronounced with the onset of activity such as getting out of bed in the morning or walking after a brief period of rest.
Swelling surrounding the injury is described as fusiform, often surrounding the entire body of the tendon.
Erythema (redness) and bruising are not common.
Many patients with a partial rupture of the Achilles tendon cannot describe an injury or single event that initiated the onset of the problem. Patients experience sharp pain at the beginning of activity, and the pain may decrease with activity. The pain may return at the conclusion of the activity. For instance, a runner may experience pain at the beginning of a run. The pain may subside during the run but return at the end of a normal running distance.
Complete Achilles Tendon Rupture
Audible pop or snap in the back of the ankle.
Unable to rise up on toes or push off at the toe-off phase of gait.
Description
A tear of the Achilles tendon can be partial or complete. Smaller, partial tears of the Achilles tendon are called micro tears. Micro tears measure a millimeter to several millimeters in size and can be single or multiple in number. Micro tears can propagate into a larger, longitudinal tear over time. Longitudinal tears can be as small as a centimeter or as large as several centimeters. Longitudinal tears of the Achilles tendon dissect the length of the Achilles tendon, paralleling the fibers of the tendon. An MRI is used to determine the presence of a tear in the Achilles tendon and whether the injury is a micro tear or larger longitudinal tear.
A complete rupture of the Achilles tendon can be debilitating. Most complete ruptures occur 2 to 4 centimeters proximal to the insertion of the tendon into the calcaneus (heel bone.) A Thompson test is used to evaluate a suspected torn Achilles tendon. With the patient lying prone, the calf is squeezed. If the patient has an intact Achilles tendon, the foot will plantarflex. This is called a negative Thompson sign. If the calf is squeezed and the foot does not plantarflex, this indicates a positive Thompson's sign and complete rupture of the Achilles tendon.
Causes and Contributing Factors
Many patients who sustain a complete tear of the Achilles tendon describe a long period of chronic Achilles tendinitis leading up to a complete rupture of the Achilles tendon. Other factors that may contribute to a partial or complete rupture of the tendon include the use of steroids (oral and injectable), the use of fluoroquinolone antibiotics (Levaquine, Cipro), smoking and advanced age.
Differential Diagnosis
The differential diagnosis of an Achilles tendon rupture includes:
Ankle fracture
Calcaneal stress fracture
Gout
Plantaris tendon rupture
Posterior tibial tendon dysfunction
Posterior shin splints
Rheumatoid arthritis
Septic arthritis
Reiter's syndrome
Retro-calcaneal bursitis
Sever's disease
Shepard's fracture
Treatment
Conservative care of partial or complete Achilles tendon ruptures includes 10 to 12 weeks in a below the knee cast. The cast is is applied to the patient in a slightly plantarflexed position, relieving tenson on the Achilles tendon. Casting can be performed in a serial manner, with less plantarflexion in each cast as the tendon heals. Additional casting in a walking cast with an elevated heel is common. Physical therapy is often recommended after casting to help the patient regain strength and flexibility.
Numerous articles in the literature compare the merits of conservative and surgical care in the treatment of partial and complete Achilles tendon ruptures. Surgical techniques vary and can be performed with either an open or minimal incision technique. Surgical repair of the Achilles tendon is performed under general anesthesia with the patient in the prone position. The damaged margins of the tear are debrided to healthy tissue. A special stitch called a Bunnell suture is used to reappose the margins of the torn Achilles tendon. A Bunnell suture includes a criss-cross of stitches to prevent tear-out of the suture. Graft tendons may be used to supplement repair. Synthetic grafting material may also be used to supplement defects in the length of the tendon. Surgical repair of the Achilles tendon may also be performed with a combination of percutaneous and open techniques. Surgical correction is always followed with non-weight-bearing casting for eight weeks. Unfortunately, re-rupture of the Achilles tendon can occur regardless of whether conservative of surgical correction is used to repair the Achilles tendon.
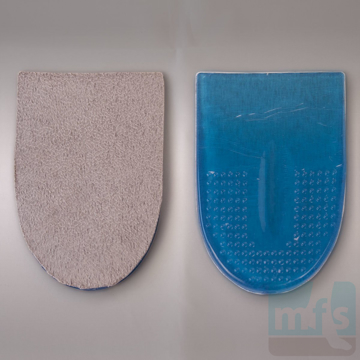
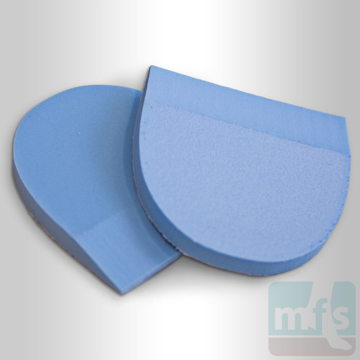
The disability following Achilles tendon surgery can be prolonged. Weakness and atrophy of the calf muscle as a result of treatment of the tear are common and can be challenging for the patient and physical therapy team. One study reported 2 centimeters of calf atrophy two years after surgery. Additional studies found persistent weakness in the calf after surgery regardless of whether conservative or surgical correction was used. Early weight-bearing and range-of-motion play important roles in how quickly a patient returns to activity. Other variables in healing include age, physical well-being of the patient prior to surgery and smoking. Return to weight-bearing is usually initiated with the use of a heel lift bilaterally. The height of the lift is reduced in the weeks after the discontinuation of casting as strength returns to the injured Achilles tendon.
When to Call Your Doctor
Symptoms of partial or complete rupture of the Achilles tendon should be promptly evaluated by your podiatrist or orthopedist.
Author
![]() This article was written by Myfootshop.com medical advisor, Jeffrey A. Oster, DPM.
This article was written by Myfootshop.com medical advisor, Jeffrey A. Oster, DPM.
Competing Interests - None
Cite this article as - Oster, Jeffrey. Achilles tendon rupture. https://www.myfootshop.com/article/achilles-tendon-rupture
Most recent article update - September 29, 2022.
 Achilles Tendon Rupture by Myfootshop.com is licensed under a Creative Commons Attribution-NonCommercial 3.0 Unported License.
Achilles Tendon Rupture by Myfootshop.com is licensed under a Creative Commons Attribution-NonCommercial 3.0 Unported License.
Internal reference only: ZoneP1, ZoneL4, ZoneM1, ZoneR1